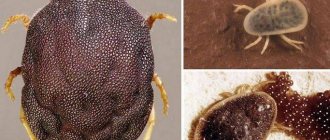
Ehrlichia - causative agents of monocytic ehrlichiosis in humans
Ehrlichia is a type of bacterial infection whose intermediate host is ixodid ticks. Infection with pathogenic microorganisms occurs when a blood-sucking insect bites and breaks the integrity of the victim’s skin.
Ehrlichia enters the human body along with the saliva of the ixodid tick. The average duration of the incubation period of infectious microorganisms ranges from 1 to 21 days, depending on the immune status of the patient. The first pronounced symptoms of the disease, which can be diagnosed as ehrlichiosis, appear 2-3 weeks after the tick bite.
The spread of ehrlichia in the human body occurs through the lymphatic channels. Together with the flow of lymph, a bacterial infection saturates the blood, and the proliferation of microorganisms occurs intracellularly and directly in the vascular endothelium.
In the process of reproduction and increase in the number of ehrlichia, multiple infectious granulomas are formed, which can also be localized in the tissues of internal organs.
Ehrlichia causes tick-borne ehrlichiosis in humans and animals
Acute and chronic foci of inflammation of bacterial etiology develop, affecting the bone marrow, liver, heart, vascular and nervous systems. Ehrlichia can parasitize the human body for several months, and if left untreated, the disease becomes chronic.
How does infection occur?
The causative agent of the disease enters a person when the tick attaches itself to the victim’s body. Ehrlichia penetrate along with the saliva of the parasite. They then spread throughout the body along with the bloodstream. The pathogen attacks white blood cells and significantly reduces the body's protective functions, suppressing the functioning of the immune system.
On a note!
Ehrlichia are gram-negative, rickettsia-like intracellular parasites that are rapidly destroyed in air. The main source of habitat is dogs and deer.
It will be possible to detect signs of infection with ehrlichiosis only after the incubation period, when a sufficient number of parasites are formed in the human body, which can significantly complicate the work of the entire body. Proper treatment will quickly stop the proliferation of the pathogen and cure the person.
Probability of infection
In humans, tick-borne ehrlichiosis can develop after being bitten by one or several ixodid ticks, which were carriers of bacterial microorganisms - ehrlichia.
Predisposing factors to the development of the disease are the presence of chronic diseases of internal organs, severely weakened immunity, abuse of alcoholic beverages, drugs, smoking, heavy physical and mental work, which weaken the body's protective functions.
On average, out of 57 ixodid ticks, 19 blood-sucking insects are infected with ehrlichia.
The pathogenicity of this microorganism is high. The probability that a person bitten by an infected ixodid tick will develop monocytic ehrlichiosis is 85%.
Prevention
There is no vaccination against tick-borne ehrlichiosis. Preventive measures are as follows:
- Try to limit yourself from visiting places where ixodid ticks live.
- When walking in public gardens, parks, and forests during tick season, use repellents—body and clothing sprays.
- When visiting endemic areas, wear a special protective suit.
- In case of a bite, it is correct to remove the tick using a device that can be purchased at a pharmacy, or seek help from a medical facility. It is strictly forbidden to extract the parasite using “grandmother’s methods”: vegetable oil and other liquid fractions. Suffocation of the parasite will provoke the release of its contents into the human body.
- After removing the bloodsucker, it must be placed in a jar and submitted for analysis. If ehrlichia or causative agents of other diseases (encephalitis, Lyme disease) are detected in a tick, a course of antibiotics is prescribed.
- Most experts agree that 0.1 g of Doxycycline should be taken as prophylaxis after a tick bite.
Causes of tick-borne ehrlichiosis and provoking factors
Tick-borne ehrlichiosis in humans is a disease that develops after the bite of a blood-sucking insect, or as a result of contact of open wounds and soft tissues of the body with a source of infection. Most people suffering from this disease discovered signs of monocytic ehrlichiosis 14-21 days after the tick bite.
Contact with blood-sucking insects most often occurs in the wild (hiking, hunting, fishing, active recreation in the forest). Low-growing shrubs and dense grass along trails and dirt roads are the natural habitat of ixodid ticks, which are the primary vectors of ehrlichiosis.
In addition to the traditional and most common mechanism of infection of the human body with Ehrlichia, the following predisposing factors for the spread of bacterial infection can be identified.
Skin rash
Areas of the skin, the integrity of which is compromised as a result of the formation of a rash or scratching, are open gates for the penetration of ehrlichia. Infection can occur in the wild, public transport, or in a hospital infectious disease department where sanitary and hygienic standards are not observed.
Weak immunity
Children and adults who initially have a weakened immune system are at particular risk of contracting tick-borne ehrlichiosis. In patients in this category, the incubation period for the development of pathogenic microorganisms proceeds 2 times faster, and the clinical picture of the disease is more pronounced and has signs of an acute inflammatory process.
Weakening of the protective functions of the immune system can occur for the following reasons:
- poor and unbalanced nutrition;
- hard mental and physical labor;
- stressful situations and nervous breakdowns;
- long-term therapy with antibacterial agents;
- the presence of other chronic diseases of bacterial etiology.
People who have previously undergone surgery or have been treated with chemotherapy drugs are also at risk of developing tick-borne monocytic ehrlichiosis.
Organ transplantation and blood transfusion
Tick-borne ehrlichiosis in humans is a disease that can be contracted without visiting forested areas or other wild environments. One of the causes of Ehrlichia infection is blood transfusion and transplantation of internal organs from a carrier of pathogenic microorganisms to a healthy person who requires donor assistance.
In this case, the source of monocytic tick-borne ehrlichiosis are people who were previously bitten by a blood-sucking insect and did not undergo full treatment, which resulted in the development of a chronic form of the disease.
Undifferentiated treatment of zooanthroponotic meningitis
In general hospitals (district, small city), in the vast majority of cases, we are not able to establish in the early stages the exact etiology of the disease that developed after a tick bite.
Some experts recommend: if after a tick bite the patient shows signs of an infectious disease (headache, hyperemia, manifestations of meningitis), early treatment should be started, simultaneously directed against the most likely causes - Lyme disease, tick-borne encephalitis, human monocytic ehrlichiosis, tick-borne rickettsiosis, human granulocytic anaplasmosis.
Strict bed rest
It is recommended, if possible, to limit the patient’s active movements as much as possible, including during intrahospital transportation. There is evidence that these simple measures can improve the prognosis of the disease with tick-borne encephalitis.
Artificial pulmonary ventilation (ALV)
In patients with profound disturbances in the level of consciousness and respiratory failure, artificial ventilation must be used. To facilitate patient care, and due to the lack of prospects for rapid regression of the disease, early tracheostomy is recommended. The choice of ventilation mode is determined by the clinical situation.
Intracranial hypertension
One of the reasons for impaired consciousness in a patient diagnosed with meningoencephalitis may be the development of intracranial hypertension (ICH). We cannot say this for sure, since continuous monitoring of intracranial pressure was not carried out, but the administration of osmotically active drugs (mannitol 20%, sodium chloride 7.5%) according to standard regimens led to a decrease in the depth of disturbance of consciousness in some patients. As a rule, osmotically active drugs had to be used for several days. And in one case – over 2 weeks. It is possible that the effectiveness of the above-mentioned treatment methods (prescription of corticosteroids, antipyretics) is partly associated with a decrease in the incidence of ICH development.
Correction of convulsive syndrome
For emergency treatment, benzodiazepines (diazepam 10 mg IV) or barbiturates (sodium thiopental 100-200 mg IV) are used. After this, the patient is prescribed oral medications. Depending on the symptoms that appear (nature of seizures, blood pressure level, etc.), use carbamazepine (Finlepsin) enterally 200 mg 2-3 times per 24 hours, or benzobarbital (Benzonal) 100-200 mg 2-3 times day, or valproic acid (Depakine) 300-500 mg 2-3 times every 24 hours. Treatment with anticonvulsants often has to be carried out for a long time – over weeks or months.
Symptoms of monocytic ehrlichiosis
Tick-borne ehrlichiosis in humans is a disease whose initial stages resemble most other infectious diseases.
Adults and children infected with bacterial microorganisms from the Ehrlichia family experience the following symptoms:
- increased body temperature, which reaches 37-39 degrees Celsius or more;
- general physical weakness and chronic fatigue syndrome;
- fever and chills;
- the formation of red rashes on the surface of the skin (this sign of the disease is most pronounced near the site of infection in the epithelial tissue);
- complete or partial refusal to eat food associated with loss of appetite, nausea and vomiting;
- rapid loss of body weight (there is a real risk of developing anorexia).
Cough, diarrhea, attacks of cramping pain in the abdominal cavity, pharyngitis and inflammation of the laryngeal mucosa occur much less frequently.
The lack of adequate treatment or the presence of a severely weakened immune system can lead to the development of a severe form of tick-borne monocytic ehrlichiosis, which is accompanied by impaired breathing, changes in the biochemical and clinical composition of the blood, and dysfunction of the central and peripheral nervous systems.
Neurological manifestations
Tick-borne ehrlichiosis in humans is a disease whose progression disrupts the functioning of brain centers, which in turn leads to the following neurological manifestations:
- loss of physiological ability to navigate the surrounding space;
- pathological fear of direct sunlight, when a sick person develops real photophobia and panic fear of well-lit areas of the street;
- neck stiffness appears;
- sudden onset muscle spasms of the lower extremities, as well as abnormal electrical activity in the brain tissue, which can also cause epileptic seizures;
- onset of coma;
- the appearance of shortness of breath, a feeling of lack of air and other dysfunctions of the act of breathing associated with disruption of the process of nervation of the muscles responsible for the functioning of the lungs and bronchial tree;
- too active reflex reactions to external stimuli;
- impaired coordination of the upper limbs when performing movements that require precise actions;
- complete or partial palsy of cranial nerves;
- dysfunction of motor activity of muscle fibers (as a result of damage to the central and peripheral nervous systems, dysfunction of one or a complex of muscles may occur);
- the formation of single or multiple cysts, as well as malignant brain tumors that disrupt the functioning of its centers.
The occurrence of neurological disorders provoked by monocytic tick-borne ehrlichiosis is a sign that the disease is in a complicated form, and the numerical population of bacterial microorganisms has reached its peak of development. This condition of the central and peripheral nervous systems can threaten the life of a sick person.
Differential diagnosis
To exclude the presence of other diseases of inflammatory-infectious etiology in the patient, differential diagnosis is carried out. A sick person donates venous blood, which is subjected to biochemical analysis.
The main task of doctors is to isolate a strain of bacterial microorganisms from the Ehrlichia family, or other bacterial pathogens that provoked the pathological condition of the patient’s body. An infectious disease specialist deciphers the results of differential diagnosis.
Diagnosis of monocytic ehrlichiosis
In order to confirm or refute the presence of tick-borne ehrlichiosis, the patient must be examined by an infectious disease specialist or therapist, as well as undergo the following types of tests.
| Type of diagnostic examination | Purpose of analysis |
| Clinical study of capillary blood | This type of analysis allows you to determine the qualitative and quantitative composition of blood. With tick-borne ehrlichiosis, changes in the cellular composition of the blood develop that resemble signs of leukocytopenia and thrombocytopenia. Based on the results of a clinical study of capillary blood, the attending physician receives preliminary information about the severity of the inflammatory process and the extent of insemination of the body by a bacterial infection. |
| Biochemical analysis of venous blood | Bacterial microorganisms from the Ehrlichia family are identified in venous blood. A comparative analysis is also performed for the possible presence of other infections that can also cause symptoms resembling tick-borne ehrlichiosis. The key symptom of this disease is a sharp increase in liver enzyme levels. Doctors also have the opportunity to isolate the bacterial causative agent of ehrlichiosis. |
| Smear from the mucous membrane of the larynx | Bacteriological examination of a smear collected from the mucous membrane of the larynx shows the composition of the microflora of this part of the body, and also makes it possible to exclude infectious diseases of the upper respiratory tract, tonsils, and larynx. For example, if the development of tick-borne ehrlichiosis is accompanied by abnormal symptoms, and its first manifestations resemble pharyngitis or ARVI. |
| Bacteriological examination of tissue in the area of a tick bite | Epithelial and soft tissues that have been bitten by a tick contain the maximum concentration of ehrlichia. Especially if a smear from an open wound was taken in the first 10-15 minutes. after removing the blood-sucking parasite from the body. This diagnostic research method can also be used as a prophylactic method to detect infection in a timely manner and prevent further development of a severe form of the disease. |
To reduce the risk of developing monocytic tick-borne ehrlichiosis, as well as to prevent the onset of the disease, it is recommended to seek medical help immediately after a tick bite.
The blood-sucking insect, which was removed from the body, is also given to doctors, who send it to specialists of the sanitary and epidemiological service for examination for infection with bacterial microorganisms from the Ehrlichia family.
Diagnosis of ehrlichiosis
Ehrlichiosis can be difficult to diagnose because the patient may not know they have been bitten by a tick and the symptoms are similar to other illnesses such as the flu.
A blood test can show the presence of antibodies that develop in response to a tick bite. However, antibodies usually appear a week after the bite.
The doctor orders laboratory tests to check:
- Increased levels of liver enzymes;
- Decreased platelet count;
- Decrease in the number of leukocytes.
If symptoms last longer than 7 to 10 days, your doctor may order a test for antibodies to Ehrlichia bacteria.
Other methods of testing for ehrlichiosis include the indirect immunofluorescence reaction (RIF). This method is rarely used and requires multiple blood samples at different times to test the body's immune response.
Indications for consultation with other specialists
The main specialist who deals with the treatment of monocytic tick-borne ehrlichiosis is an infectious disease doctor. If there is no doctor of this profile in the district clinic, then his responsibilities are assigned to the therapist.
Patients who have not sought medical help for too long, self-medicated, or suffer from a complicated form of the disease may require consultation with the following specialists:
- neurologist;
- cardiologist;
- pulmonologist;
- hematologist;
- hepatologist
The need to involve doctors of other specializations is determined individually by an infectious disease specialist based on the results of an initial examination and a more thorough diagnostic examination of the body.
How to treat tick-borne ehrlichiosis
60–70% of patients are urgently hospitalized and undergo an intensive therapeutic course in a hospital setting. For mild to moderate severity of tick-borne ehrlichiosis, treatment is carried out on an outpatient basis.
Patients are prescribed the following drugs:
- To eliminate the cause of the disease, tetracycline antibiotics are used. Mostly, Doxycycline 100 mg every 1 hour. For a child, the dosage is 2.2 mg/kg body weight twice a day. Tetracycline and Levomecitin can also be used. Alternatively, Chloramphenicol, Rifampicin.
- To eliminate symptoms, antipyretic and painkillers are prescribed, and for detoxification, glucose-saline solutions are prescribed intravenously.
- To relieve symptoms, the use of vitamins, antispasmodics, irrigants for the oral and nasopharyngeal mucosa, and anti-diarrhea medications is indicated.
With proper therapy, improvement occurs within 24–72 hours, depending on the severity of the disease. The course of treatment lasts from 7 to 14 days.
If you are pregnant and allergic to Doxycycline, your doctor may prescribe a treatment regimen with alternative drugs: Rifampicin, Chloramphenicol.
Treatment options
Therapy for tick-borne ehrlichiosis involves the systemic administration of antibacterial drugs, the active components of which disrupt the pathogenic activity of infectious microorganisms.
Conservative therapy
Drug treatment of tick-borne ehrlichiosis is carried out using the following tetracycline antibiotics.
Vibramycin D
This is a complex antibacterial drug, 1 tablet of which contains 106.045 mg of doxycycline monohydrate. When treating tick-borne ehrlichiosis, the medication is prescribed to take 1 tablet 3 times a day with meals. The course of therapy is from 10 to 14 days. The drug is contraindicated for children and women who are pregnant.
Tetracycline hydrochloride
1 tablet of the drug contains 100 mg of tetracycline hydrochloride. The medication is indicated for use in the treatment of inflammatory processes caused by bacteria sensitive to its active component.
The recommended dosage is 2 tablets every 6 hours. The drug is taken 1 hour before meals and is contraindicated in patients prone to allergic reactions to tetracycline antibiotics.
Doxycycline
1 capsule of this medication contains 100 mg of the active substance - doxycycline chylate. The drug suppresses the pathogenic activity of bacteria from the Ehrlichia family, promoting their death. Take 1 tablet 2-3 times a day after meals. The course of treatment is at least 10 days. It is contraindicated in patients with severe liver failure.
These are basic medications that are indicated for patients diagnosed with tick-borne ehrlichiosis. The treatment regimen for complicated forms of the disease is developed individually, depending on which organs and systems are affected by the pathogenic activity of ehrlichia.
Experimental treatment
Bacteria from the Ehrlichia family are infectious microorganisms, the treatment of which involves taking drugs whose active components are tetracycline and doxycycline. In combination with these medications, medications are prescribed aimed at cleansing the blood of toxins produced by pathogenic microorganisms.
These are the sorbents Activated carbon, Enterosgel, Atoxil, which are used 2 hours after taking antibiotics. The required dosage is determined by an infectious disease specialist or therapist depending on the severity of the patient’s condition. This is the only way to quickly and effectively treat tick-borne ehrlichiosis.
Treatment of ehrlichiosis
Ehrlichia is sensitive to tetracycline antibiotics. In most cases, they prefer to treat the patient with Doxycycline. The use of chloramphenicol is also allowed.
The procedure for treatment with various antibiotics after a tick bite:
- Tetracycline: 0.3-0.4 g 4 times a day.
- Doxycycline: 0.1 g twice a day in the first 24 hours, subsequent days single dose.
If the patient is allergic to tetracycline antibiotics, he is treated with Rifampicin, the average course of treatment is 7-10 days. A shorter duration is not advisable even with a clear improvement in the patient's condition.
Important!
According to statistics, the mortality rate from monocytic ehrlichiosis in humans is up to 5%, with granulocytic ehrlichiosis up to 10%. Data are based on studies in the USA,
With the development of complications and acute course of the disease, the participation of specialized specialists is required to stabilize the patient’s condition.
To alleviate the patient's condition, various antipyretics may be prescribed. Most often I use Paracetamol or Ibuprofen for this purpose.
The prognosis largely depends on the timeliness of the treatment started, as well as the initial state of the body. It will be more difficult to cure a person with a weakened immune system, low levels of platelets and leukocytes.
When starting therapy in the early stages of the disease, the patient feels relief within 48 hours. After recovery, the body develops strong immunity, which lasts for 2 years.
Treatment of monocytic ehrlichiosis in humans
Complications and prognosis
Monocytic tick-borne ehrlichiosis is a dangerous disease that can be completely cured within 2-3 weeks. This favorable prognosis for recovery is possible only if you go to the hospital in a timely manner, when the tick bite has just occurred, or in the first 1-2 days after the onset of symptoms of the disease.
Lack of diagnostic examination and qualified treatment can lead to the following complications:
- single or multiple brain cysts;
- infectious liver hepatitis;
- a radical change in the biochemical composition of the blood, a decrease in platelet levels and impaired blood clotting;
- chronic inflammation of bronchopulmonary tissue;
- bacterial meningitis;
- the development of internal bleeding in the organs of the gastrointestinal tract (men and women who suffer from a concomitant disease in the form of stomach ulcers are at particular risk);
- inflammation of the spinal cord;
- paralysis of individual parts of the body;
- dysfunction of the musculoskeletal system;
- inflammatory damage to nerve endings;
- various dysfunctions of the digestive system;
- epilepsy;
- loss of ability to work and lifelong disability;
- arrhythmic disturbances in the functioning of the heart muscle.
In medical practice, there have been clinical cases where complicated forms of tick-borne ehrlichiosis caused death. An equally dangerous prognosis for the development of the disease is its transition to a chronic form with gradual destruction of the tissues of internal organs.
Clinical examination
Clinical examination of monocytic tick-borne ehrlichiosis involves an annual preventive medical examination. A routine examination includes an examination by a neurologist, therapist, or dermatologist. It is mandatory to donate blood from a finger and vein.
First of all, people living in regions with high activity of ixodid ticks, which are carriers of bacteria from the Ehrlichia family, are subject to medical examination.
Tick-borne ehrlichiosis in humans is an infectious disease transmitted by blood-sucking insects. Its main danger is that the bacterial microorganisms of ehrlichia lead an intracellular parasitic lifestyle.
Pathogenic microorganisms destroy blood vessels and tissues of internal organs, causing the formation of benign tumors. Severe forms of ehrlichiosis lead to the destruction of the central and peripheral nervous systems and also cause death.
Article design: Vladimir the Great