Etiology
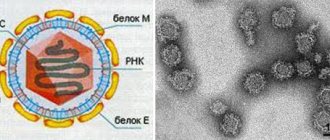
The causative agent, Rickettsia sibirica, was discovered in 1938 by O.S. Korshunova. Like other pathogens of the group of spotted fevers, it parasitizes both in the cytoplasm and in the nucleus of the affected cells. Antigenically it differs from other rickettsiae in this group. Contains a toxic substance. Characterized by properties common to all rickettsiae. Able to persist for a long time in the external environment at low temperatures (up to 3 years). Keeps well when dried. The virulence of individual strains varies significantly.
Treatment regimen
At the first suspicion of the disease, the patient is hospitalized and prescribed bed rest, which lasts until the onset of the third stage of the disease and another five days.
You are allowed to move independently around the ward only a week after the temperature has subsided. Patients do not require a special diet; they are assigned to a common table, but it is necessary to take into account his condition. Nausea and vomiting in the first days of illness can lead to lack of appetite. You should ensure that the patient eats well, receiving sufficient vitamins and essential nutrients needed by the body to fight the disease. In addition, you should reduce the load on the liver and kidneys by reducing fried, spicy and salty foods from your diet.
Important! During this period, it is necessary to maintain hygiene, keep clothes and body clean, and prevent the occurrence of bedsores. Since the patient is not able to do this on his own, he needs good care.
Typhus is treated with tetracycline antibiotics and chloramphenylcol. This gives positive results within 2-3 days. Kars treatment must be continued for another 2 days after the temperature drops to normal. Intravenous systems of detoxification solutions are prescribed, which significantly alleviate the patient’s condition 5% glucose,
Throughout the illness, the patient should be monitored not only by an infectious disease specialist, but also by a cardiologist and neurologist. Ephedrine and sedatives may be used if necessary.
In particularly severe cases, prednisolone may be used.
We can talk about final recovery only 2 weeks after the last manifestations of the disease.
Another danger: ways to detect and get rid of bed mites at home.
In what cases is Travogen used, and in what forms it is sold here in more detail.
Will Nogtivit help with nail fungus: https://parazity-gribok.ru/fungus/nails/nogtivit-ot-gribka-nogtej.html.
Epidemiology
The disease is classified as a zoonotic disease with natural focality. Natural foci have been identified in the Primorsky, Khabarovsk and Krasnoyarsk territories, in a number of regions of Siberia (Novosibirsk, Chita, Irkutsk, etc.), as well as in Kazakhstan, Turkmenistan, Armenia, Mongolia. The reservoir of rickettsia in nature is about 30 species of various rodents (mice, hamsters, chipmunks, gophers, etc.). Transmission of infection from rodent to rodent is carried out by ixodid ticks (Dermacentor nuttalli, D. silvarum, etc.). The infestation of ticks in foci reaches 20% or more. The incidence in the tick habitat ranges from 71.3 to 317 per 100,000 population per year. The immune layer of the population in natural foci ranges from 30 to 70%. Rickettsia remain in ticks for a long time (up to 5 years); transovarial transmission of rickettsia occurs. Not only adult ticks, but also nymphs participate in the transmission of infection to humans. Rickettsia is transmitted from ticks to rodents through blood sucking.
A person becomes infected during his stay in the natural habitats of ticks (shrubs, meadows, etc.), when he is attacked by infected ticks. The greatest activity of ticks is observed in spring and summer (May-June), which determines the seasonality of the incidence. The incidence is sporadic and occurs mainly among adults. Not only rural residents get sick, but also those traveling outside the city (garden plots, recreation, fishing, etc.). In recent years, about 1,500 tick-borne rickettsiosis diseases are registered annually in Russia.
Tick-borne rickettsiosis: treatment of infection
Since the disease is a bacterial infection, treatment requires the use of antibiotics. For this purpose, the drugs “Tetracycline” and “Levomycetin”, as well as their analogues, are used. In severe cases of the disease, the patient should be hospitalized in an infectious diseases hospital. For the purpose of detoxification, a solution of 5% glucose with ascorbic acid is administered intravenously. For bradycardia, it is necessary to use vasopressor drugs. These include medications “Atropine” and “Caffeine”. Symptomatic therapy is also carried out - antipyretics, antihistamines. Ticks are removed using tweezers. If complications develop, specific treatment is carried out.
Pathogenesis
The portal of infection is the skin at the site of the tick bite (rarely, infection occurs when rickettsia is rubbed into the skin or conjunctiva). At the site of introduction, a primary affect is formed, then rickettsiae move along the lymphatic pathways, causing the development of lymphangitis and regional lymphadenitis. Lymphogenously, rickettsiae penetrate into the blood and then into the vascular endothelium, causing changes of the same nature as in epidemic typhus, although they are much less pronounced. In particular, there is no necrosis of the vascular wall, thrombosis and thrombohemorrhagic syndrome rarely occur.
Endoperivasculitis and specific granulomas are most pronounced in the skin and to a much lesser extent in the brain. Allergic restructuring is more pronounced than in epidemic typhus. The transferred disease leaves a strong immunity, recurrent diseases are not observed.
Causes
The source of infection is only a sick person in the period from the last two days of the incubation period until the 7-8th day from the moment he has a normal temperature after the end of the fever.
Louse
(mainly clothes), having absorbed the patient’s blood, becomes infectious to healthy people only after 4-5 days. During this period, Provacek's rickettsia, having penetrated the digestive tract of the louse along with the patient's blood, after introducing them into the epithelial cells lining the inside of the intestinal wall, multiply in huge quantities. When the number of multiplied rickettsiae turns out to be particularly significant, the epithelial cell ruptures and the rickettsiae, along with louse feces, are excreted, contaminating the skin and underwear of the person on whose body the louse is parasitizing at the moment. By scratching the skin, a person rubs insect feces into the bite site; the rickettsiae are introduced into the human body and are included in the bloodstream. From this moment the incubation period of the disease begins.
In Tsarist Russia, especially in years of crop failure, natural disasters and during periods of war, large epidemics of typhus were observed. It is characteristic that even in the 19th century typhus epidemics affected European countries, and the number of victims of this disease often exceeded losses from military operations.
During 1918-1922. in the young Soviet country, which repelled numerous interventionists on the fronts of the civil war, a typhus epidemic arose and assumed enormous proportions; Only the system of state anti-epidemic measures made it possible to stop the spread of this infection. In 1948-1953 There were isolated cases of typhus with a predominance of mild and moderate forms of the disease; According to the clinical course, it was impossible to distinguish between primary and recurrent disease. Since 1954, typhus has been eliminated in Russia.
Symptoms and course
The incubation period ranges from 3 to 7 days, rarely up to 10 days. There are no prodromal phenomena (with the exception of the primary affect, which develops soon after a tick bite). As a rule, the disease begins acutely, with chills, body temperature rises, general weakness, severe headache, pain in muscles and joints appear, sleep and appetite are disturbed. Body temperature in the first 2 days of illness reaches a maximum (39-40°C) and then persists as a fever of a constant type (rarely remitting). The duration of fever (without antibiotic treatment) most often ranges from 7 to 12 days, although in some patients it lasts up to 2-3 weeks. When examining the patient, mild hyperemia and puffiness of the face are noted. Some patients experience hyperemia of the mucous membrane of the soft palate, uvula, and tonsils. The most typical manifestations are primary affect and exanthema. When bitten by uninfected ticks, the primary affect never develops; its presence indicates the onset of the infectious process.
The primary affect is an area of infiltrated moderately compacted skin, in the center of which necrosis or a small ulcer covered with a dark brown crust is visible. The primary affect rises above the skin level, the zone of hyperemia around the necrotic area or ulcer reaches up to 2-3 cm in diameter, but there are changes of only 2-3 mm in diameter, and they are quite difficult to detect.
Not all patients note the very fact of a tick bite. Healing of the primary affect occurs after 10-20 days. In its place there may be pigmentation or peeling of the skin. A characteristic manifestation of the disease is exanthema, which is observed in almost all patients. It usually appears on days 3-5, rarely on days 2 or 6 of illness. First it appears on the limbs, then on the torso, face, neck, and buttocks. The rash is rarely observed on the feet and palms. The rash is abundant, polymorphic, consists of roseola, papules and spots (up to 10 mm in diameter).
Hemorrhagic transformation of rash elements and the appearance of petechiae are rarely observed. Sometimes there is a “sprinkling” of new elements. The rash gradually disappears by 12-14 days from the onset of the disease. There may be peeling of the skin at the site of the spots.
In the presence of primary affect, it is usually possible to detect regional lymphadenitis. Lymph nodes are enlarged to 2-2.5 cm in diameter, painful on palpation, not fused to the skin and surrounding tissues, suppuration of the lymph nodes is not observed.
From the cardiovascular system, bradycardia is noted, a decrease in blood pressure, arrhythmias and changes in the heart muscle according to ECG data are rare. Changes in the central nervous system are observed in many patients, but do not reach the same extent as occurs with epidemic typhus.
Patients are bothered by severe headaches, insomnia, patients are inhibited, agitation is observed rarely and only in the initial period of the disease. Mildly expressed meningeal symptoms are very rarely detected (in 3-5% of patients); when examining cerebrospinal fluid, cytosis usually does not exceed 30-50 cells in 1 μl. There are no pronounced changes in the respiratory system. Enlargement of the liver is observed in half of the patients, the spleen increases less frequently (in 25% of patients), the increase is moderate. The course of the disease is benign. After the temperature drops to normal, the patients' condition quickly improves and recovery occurs quickly. Complications, as a rule, are not observed. Even before the use of antibiotics, the mortality rate did not exceed 0.5%.
Mechanism of development and symptoms of pathology
The causative agents of the disease, rickettsia, have the structure of a microorganism. But, like a virus, they are capable of intracellular parasitism. They are extremely unstable in the external environment. They die quickly when exposed to disinfectants and high temperatures. But they can survive freezing and drying.
Pathogenic rickettsiae are most often transmitted by the bite of infected ectoparasites. Some diseases in this group are characterized by airborne and nutritional infection. Factors contributing to infection include:
- Contact with sick people.
- Contact with farm animals. The feces and urine of sick cows pose a danger to humans. For this reason, tick-borne rickettsiosis occurs quite often among farm workers.
- Lack of personal hygiene.
The disease begins to develop a few days after the bite of the parasite vector. The duration of the incubation period depends on the type of pathogen and human immunity.
First, a local reaction develops: the bite site is sore, the skin area turns red and swells. Bacteria enter the lymph nodes, begin to multiply and settle there for some time. This leads to a noticeable enlargement of the lymph nodes.
A few days after infection, bacteria from the lymphatic system enter the bloodstream. Toxinemia develops. The blood vessels of the skin are affected, and an inflammatory reaction develops in their walls. Often the infection gets into the veins and arteries of the brain. In this case, the development of meningitis, encephalitis and other pathologies of the central nervous system is possible.
The incubation period can last for two to seven days. The disease most often develops acutely. The bite site thickens, a brown crust appears in its center, then redness and pain appear. Two to three days after this, the following symptoms of rickettsiosis appear:
- weakness;
- decreased blood pressure, bradycardia;
- headache;
- enlarged lymph nodes;
- lack of appetite;
- body aches;
- nausea and vomiting;
- chills and fever above 39 degrees;
- stomach ache;
- profuse rash on the extremities, which quickly spreads to the torso and face;
- damage to the nervous system;
- a 15% decrease in hemoglobin levels.
The disease is most severely affected by older people. In children it occurs more easily than in adults, but in a more acute form. Pathology has three degrees of severity. The most severe form is characterized by severe intoxication, a temperature reaching 41 degrees and a long febrile period. Complications such as bronchitis, myocarditis and pyelonephritis are possible.
Diagnosis and differential diagnosis
Epidemiological prerequisites (stay in endemic foci, seasonality, tick bites, etc.) and characteristic clinical symptoms in most cases make it possible to diagnose the disease. Primary affect, regional lymphadenitis, profuse polymorphic rash, moderate fever and benign course are of greatest diagnostic importance.
It is necessary to differentiate from tick-borne encephalitis, hemorrhagic fever with renal syndrome, typhoid and typhus, tsutsugamushi fever, syphilis. Sometimes in the first days of the illness (before the appearance of the rash), an erroneous diagnosis of influenza is made (acute onset, fever, headache, facial flushing), but the absence of inflammatory changes in the upper respiratory tract and the appearance of a rash make it possible to refuse the diagnosis of influenza or acute respiratory infections.
Epidemic typhus and tsutsugamushi fever are much more severe with pronounced changes in the central nervous system, with hemorrhagic transformation of the elements of the rash, which is not typical for tick-borne typhus in North Asia. With syphilis, there is no fever (sometimes there may be a low-grade temperature), signs of general intoxication, a profuse, polymorphic rash (roseola, papules), which persists for a long time without much dynamics. Hemorrhagic fever with renal syndrome is characterized by severe kidney damage, abdominal pain, and a hemorrhagic rash.
To confirm the diagnosis, specific serological reactions are used: RSK and RNGA with diagnosticums from rickettsia. Complement-fixing antibodies appear from 5-10 days of illness, usually in titers of 1:40-1:80 and subsequently increase. After the illness, they persist for up to 1-3 years (in titers 1:10-1:20). In recent years, the indirect immunofluorescence reaction has been considered the most informative.
CAUTION – PEDICULOSIS!
Pediculosis (lice) is a parasitic skin disease caused by a louse, a small insect that parasitizes the skin and clothing. Three types of lice (head, body and pubic) can infest humans. Pediculosis manifests itself mainly as itching at the site of lice bites (itching of the scalp, itching in the genital area).
Causes of pediculosis.
As a rule, pediculosis develops under unfavorable environmental conditions (large groups of people, lack of basic hygienic conditions, social disasters). Lice can also occur in clean people when they come into contact with a person infected with lice.
Head lice.
The cause of head lice is the head louse. Head lice live up to 40 days. Over the course of 35 days, the louse lays up to 10-12 eggs (nits) per day. Typically, nits are attached to the hair and look like transparent round sacs filled with liquid.
After emerging from the egg (nit), the young louse begins to feed on human blood and grow. Bright pigmentation is visible on the sides of head lice. The presence of head lice indicates a poor hygienic environment in the team, as well as the uncleanliness of people.
Head lice live on the scalp and are most common in girls and women, as they survive better in long hair. As a rule, lice infestation occurs through combs, hats, and hair brushes. It is also possible for the parasite to transfer from one person to another.
Head lice are extremely agile and capable of jumping high.
It may take several weeks from the moment of infection with lice (pediculosis) to the first signs of the disease.
The main symptoms and signs of pediculosis:
- Itchy skin at the site of the louse bite. With head lice, patients are most often bothered by itching of the scalp (behind the ears, in the temples and back of the head). With mild head lice, patients complain of mild itching or only slight discomfort in the area of the lice bite.
- Rash. As a rule, a rash with lice appears a few days after lice bites. Head lice is characterized by red spots along the periphery of the scalp.
- Scratching (excoriation). With long-term lice, due to itching, the patient combs the areas of skin bitten by lice. As a rule, purulent crusts appear at the site of scratching due to lice.
- The presence of nits in the hair. The presence of nits on the hair is one of the irrefutable signs of lice. Nits appear as small (2-3 mm) silvery bubbles attached to the hair. Nits can be live or dead. Dead nits are usually dull in color.
Complications of pediculosis:
- Pyoderma, impetigo - a secondary bacterial infection - a skin disease caused by the introduction of pyogenic microbes into the skin; characterized by the appearance of superficial vesicular-pustular rashes on the scalp, behind-the-ear areas, and face.
- Blepharitis, conjunctivitis - inflammation of the eyelid area and mucous membrane of the eyes.
- Lymphadenitis is inflammation of the lymph nodes.
- Sepsis is a blood poisoning, a serious disease that is accompanied by disruption of all organs and poses a threat to the patient’s life.
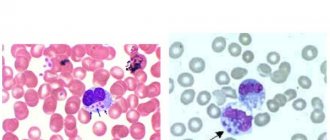
- Typhus (epidemic) is an acute infectious disease (rickettsiosis), the causative agent of which is the intracellular parasite Rickettsia Provachek. The carriers of rickettsia are mainly lice, mainly body lice, less often head and pubic lice. The main mechanism of infection is transmissible (through insect bites - lice, as well as fleas). The source of infection is a person suffering from epidemic typhus or Brill's disease. When sucking blood, rickettsiae enter the digestive system of lice along with the patient's blood, which, having multiplied in the intestinal epithelium of the lice, are excreted in their feces already 4 days after infection by the lice. From this moment, lice become infectious and, when biting a healthy person, are able to infect him, releasing feces containing pathogens near the site of blood sucking. Scratching the itchy bite area, a person rubs rickettsiae into the wound. The incubation (latent) period of the disease lasts from 6 to 25 days. The disease is characterized by destructive changes in the inner wall of blood vessels (endothelium) and the development of thrombus formation - generalized thrombovasculitis. Epidemic typhus is characterized by: the presence of patients with pediculosis, seasonality and focality.
Clinical manifestations of typhus are varied and associated with rickettsia (penetration of the pathogen into the bloodstream), damage to blood vessels, the nervous system and are characterized by general intoxication, fever, the appearance of roseola-petechial rash, the presence of “typhoid status” (mental disorders manifested by psychomotor agitation, talkativeness , sometimes memory disorders; insomnia progresses; shallow sleep is accompanied by dreams of a frightening nature, which is why patients are sometimes afraid to fall asleep; disorientation of patients is often observed; delusions, hallucinations, loss of consciousness are possible).
Highlight:
- Complications associated with vascular damage characteristic of typhus: thrombosis, thromboembolism, thrombophlebitis, endarteritis, rupture of cerebral vessels, damage to the nuclei of cranial nerves, polyradiculoneuritis, intestinal bleeding, myocarditis, heart attack, inflammation of the brain (meningoencephalitis); damage to the central nervous system - collapse, psychosis during convalescence and later; the occurrence of bedsores and gangrene of the distal extremities. Critical conditions are caused by infectious-toxic shock, pulmonary embolism.
- Complications caused by secondary bacterial infection: secondary pneumonia, otitis media, mumps, abscesses, furunculosis, pyelitis, pyelocystitis, stomatitis, phlegmon of the subcutaneous tissue.
- Brill's disease (relapsing typhus). The causative agents of typhus (rickettsia) can remain viable for a long time in a latent (hidden) state in the cells of the immune system of a person who has previously had epidemic typhus. Relapses of the disease are possible after many years and are caused by internal (endogenous) factors of the body, without external influences. In this case, the disease occurs sporadically (in the form of isolated, unrelated cases) and the source of infection is the patient himself.
The dominant role belongs to the physiological state of the body. Activation of infectious agents occurs when the activity of the human immune system decreases under the influence of external and internal factors, which include: stress; physical overload; severe somatic diseases; hypothermia; immunodeficiency states; malnutrition and other factors.
With the weakening of the restraining influence of immune defense factors, the pathogen enters the blood, infects vascular endothelial cells and triggers a cascade of pathological reactions, as in the primary infection of epidemic typhus; but in this case the concentration of the pathogen in the blood is much lower. Activation of a latent infection leads to the development of an endogenous relapse of the disease - Brill's disease , in which rickettsiae re-enter the bloodstream and damage blood vessels, determining the patient's infectiousness.
The incidence of Brill's disease is recorded both in places of former typhus epidemics and in areas free from this infection (in persons arriving from disadvantaged areas). This pathology affects elderly or senile people who once experienced a typhus epidemic. It should be noted that if there is lice, the patient can be dangerous to others.
Complications of this disease develop in rare cases, most often these are pneumonia, which is characteristic of the addition of a secondary infection and thrombophlebitis - mainly in older people.
Prevention of head lice:
Prevention of pediculosis involves the use of a set of measures to combat the spread of the disease:
- Conducting a systematic, personal examination of the scalp. Timely completion and conduct of routine medical examinations - when visiting a local doctor and staying in organized groups.
- If parasites are detected, you must immediately seek medical help from a specialist at a medical institution and begin effective treatment according to an individual course developed and prescribed by a doctor. Self-medication is unacceptable! After recovery, you should remember to continue to follow the necessary measures to prevent head lice!
- Conducting a timely mandatory medical examination of all contact persons and organizing medical observation of contact persons - within the time limits established by the legislative and organizational and methodological documents of the Ministry of Health of the Russian Federation, the Office of Rospotrebnadzor of the Russian Federation, the Office of Rospotrebnadzor for the city of Moscow, the Department of Health of the city of Moscow.
- Establishment of quarantine (restrictive) measures in organized teams.
- Immediate referral of persons infected with pediculosis pubis to the skin and venereal disease clinic at their place of residence.
- Maintain personal hygiene. It is necessary to change underwear and clothes regularly (at least 2 times a week). It is also important to constantly wash bedding at high temperatures (you should avoid using other people's bedding and clothing). You should iron your clothes carefully (especially in the seam area).
- Constant implementation of hygienic measures to prevent insect contamination of the surrounding area:
- mandatory and regular body washing;
- change of bed linen every 7-10 days;
- systematic hair care (combing, cutting);
- use only your personal comb when caring for your hair;
- regular washing of clothes and bedding;
- Carrying out regular cleaning of all indoor premises and adjacent areas;
- constantly maintaining the cleanliness of all environmental items in the premises and surrounding areas;
- mandatory training of children in hygienic training skills to prevent their infection with head lice.
The fight against pediculosis (lice) continues to be a pressing problem in protecting human health and is important in the prevention of health-threatening infections caused by parasites.
Remember, it is necessary to constantly fight against pathogenic insect parasites!
Your health and the health of your child, your family is in your hands!
Preventive measures
Knowing the epidemiology of typhus, prevention can be quite simple: combating head lice. This is the main method of protection against this disease. It is important to maintain personal hygiene, promptly wash clothes in water above 60°C, and also iron underwear.
If a sick person is identified, his personal belongings must be destroyed and household items must be thoroughly disinfected.
If you are at the source of the disease or in forced contact with a patient, you should undergo a ten-day course of treatment with tetracycline antibiotics.
The video details the causative agent of typhus:
Complications and prognosis
Complications after tick-borne rickettsiosis are usually very severe, and are provoked by the effects of pathological processes on the central nervous system, musculoskeletal system, cardiovascular, pulmonary systems, skin and kidneys.
Main complications:
- Hypovolemia.
- Electrolyte disturbances.
- Peripheral gangrene.
- Secondary infections, especially bacterial pneumonia.
Without treatment, death can occur in 10-50% of patients with epidemic tick-borne typhus, 4-40% with tsutsugamushi and about 2% with endemic typhus.
Regarding prognosis, uncomplicated cases that are promptly diagnosed and treated very well are usually associated with complete recovery.
Complex or delayed variants have a higher risk of complications, but are still generally quite treatable, depending on comorbidities and the degree of immunity of the patient.
Before the advent of antibiotics, the mortality rate of typhus reached 60%. The highest mortality rate occurs in adults, especially in elderly and malnourished patients.
Without treatment, death can occur in 10-50% of patients with epidemic tick-borne typhus, 4-40% with tsutsugamushi and about 2% with endemic typhus.