Description of tick-borne rickettsiosis
Tick-borne rickettsiosis is an infectious pathology characterized by skin manifestations, widespread vasculitis and intoxication syndrome. The disease is characterized by transmissible transmission. The infection is carried by ticks and lice. There are several variants of the course of rickettsiosis. The main difference between these pathologies is the type of pathogen. Some rickettsioses are common in steppe and desert areas, others in tropical climates. Nevertheless, all these pathologies have a similar clinical picture. The disease can be suspected based on characteristic symptoms, as well as epidemiological characteristics. The main diagnostic method is serological testing, which allows you to accurately determine the type of pathogen.
Diagnosis and treatment
Tick-borne rickettsiosis is diagnosed by taking a patient's blood for a serological test, which will show whether there is DNA or RNA of the virus in their blood. A bacteriological study is also indicated to identify the causative agent of infection. The pathogen can be isolated from the patient’s blood, from the place of its primary localization. Skin allergy tests are often used to make a diagnosis. Differential diagnosis is important, including meningococcal infection, measles, influenza and other viral diseases.
If we talk about treatment, it will vary in each individual case. The main drug used to treat rickettsial infections is an antibiotic. Depending on the clinical manifestations of the disease, symptomatic therapy may be required. In particular, smallpox rickettsiosis also requires local treatment, which will consist of treating scabs that have formed on the skin and removing dead tissue. The process of treating the disease is long. It is important that a qualified specialist constantly monitors the patient's condition.
During treatment, it is mandatory to protect medical personnel from the spread of pathogens. Therefore, employees must wear special protective suits and perform all manipulations in strict accordance with safety rules.
In some cases, such as Q fever or a form such as vesicular rickettsiosis, immunization is indicated to prevent the spread of infection. Treatment of patients with this disease is carried out in infectious diseases hospitals in special boxes, which helps prevent the spread of infection.
As mentioned above, only a few forms of this pathology pose a serious danger to humans - most, including vesicular rickettsiosis and tick-borne rickettsiosis, occur without complications, so the recovery process occurs quite quickly (after starting treatment with antibacterial agents).
Prevention of infection with such pathologies involves the fight against ticks, lice and other insects that can become carriers. Also, great importance in prevention is given to deratization - the destruction of accumulations of mice and rats in the basements of buildings, in sewers and landfills.
What to do?
If you think you have Rickettsial disease
and the symptoms characteristic of this disease, then an infectious disease doctor can help you.
Source
Did you like the article? Share with friends on social networks:
What types of rickettsial diseases exist?
As you know, rickettsioses are a large group of diseases. They are distributed all over the world. The most common types are considered to be:
- Rickettsia prowazekii – this pathogen causes typhus. This disease is transmitted transmissibly (through lice bites).
- Rickettsia typhi is the causative agent of endemic typhus. It is transmitted by rodent and flea bites.
- Rickettsia sibirica. This pathogen causes the disease North Asian tick-borne rickettsiosis.
- Rickettsia burneti. When this pathogen enters the human body, Q fever develops. The disease is transmitted transmissibly through the bites of ixodid ticks.
- Rickettsia orientalis. Like previous types of rickettsioses, this pathology is transmitted by tick bites.
READ ALSO: Rash between the fingers of a child; How to cure allergies
In addition to the listed diseases, there are many more infections caused by various strains of this pathogen.
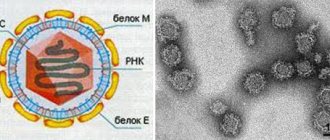
Pathogen
The causative agent of North Asian tick-borne rickettsiosis is Rickettsia sibirica. The bacterium belongs to the group of pathogens of tick-borne spotted fever based on its cytomorphological and seroimmunological characteristics. Rickettsia sibirica is characterized by intranuclear and cytoplasmic localization, as well as other representatives of this group of rickettsia - R. conori, R. rickettsi, R. murinus.
In the first phase of the infectious process (infection phase), rickettsiae enter the human body due to disruption of the skin when the vector tick is attached. Following the introduction of the pathogen, it multiplies at the entrance gate, resulting in the development of primary affect. It is a dense infiltrate, covered with a brown crust with an area of necrosis in the center. Proliferative dermatitis develops at the site of tick suction. Morphological and histological examination of the tissue at the site of the primary affect in the cytoplasm of exudate cells, in the vascular endothelium and histiocytes reveals rickettsiae.
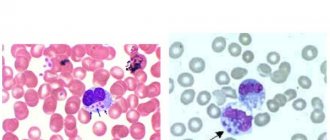
In the second phase of the infectious process - lymphogenous introduction, rickettsiae enter regional lymph nodes through the lymphatic ducts. Changes of a destructive-proliferative nature occur in the lymphatic vessels. Acute lymphadenitis and periadenitis are observed in the lymph nodes. In addition to the lymphatic system, rickettsiae spread through the venous vessels, resulting in hematogenous dissemination. Rickettsia and toxemia develop, and after 2-4 days the general symptoms of the disease appear. As a result of the toxic effect of rickettsiae, the regulatory function of the central nervous system is disrupted, the walls of blood vessels are affected, and a rash quickly appears. Histological changes in the affected areas consist of proliferative and destructive phenomena.
With North Asian tick-borne rickettsiosis, significant proliferative vascular changes are observed, the neurohumoral regulation of vascular tone is disrupted, leading to dystonia and hypotension. As with other rickettsioses, the effect of the allergic component manifests itself, expressed in granulomatous vascular lesions.
Of great importance in the pathogenesis are vascular changes in the brain, which are expressed in endovasculitis, destructive thrombovasculitis in the smallest arterioles and capillaries. They lead to significant disorders of the nervous system. In addition, toxic changes are observed in the liver, heart muscle, kidneys and other internal organs.
In the subsequent phase of growth of specific immunity, the body is freed from the pathogen and recovery occurs.
Epidemiological characteristics of rickettsioses
Rickettsioses differ from each other not only in the type of pathogen, but also in epidemiological characteristics. Despite its wide prevalence throughout the world, each disease is common in a specific area. For example, epidemic typhus is also called prison or ship fever, since this pathology is transmitted through lice bites, which were widespread among prisoners and sailors. A similar disease, but caused by the pathogen Rickettsia typhi, is more often recorded in regions with warm climates. It is especially common in rural areas in the summer.
Tick-borne rickettsiosis is common in the habitats of these insects. This group of infectious pathologies is found in Northern Asia, Japan, Australia, and mountainous regions. Most rickettsioses are zoonotic diseases. Wild and domestic animals and rodents are considered an intermediate reservoir of infection. Various types of ticks are carriers of rickettsiosis. Since these insects breed in the summer (May-September), during this period the incidence increases sharply. Most often, the infection affects people who work outdoors (dachas, gardens, pastures) and come into contact with animals.
Methods of infection
Rickettsia are intracellular parasites that cause acute febrile conditions in humans. In total, 29 species of rickettsia are known. Each bacterium can cause the development of a certain type of rickettsiosis. Moreover, the characteristics of all pathologies are similar.
The most commonly recorded types of human rickettsial infections are:
- Rickettsia prowazekii. It causes the development of typhus. The infection is transmitted through body lice bites.
- Rickettsia burneti. Penetrating into the body, the pathogen causes the development of Q fever. The carriers are ixodid ticks.
- Rickettsia typhi. Endemic typhus. Can be transmitted through flea and rodent bites.
- Rickettsia orientalis. The bacterium causes the development of Tsutsugamushi disease. The carrier is the red mite tick.
- Rickettsia sibirica. The causative agent of North Asian tick-borne rickettsiosis.
These pathogens are also responsible for the development of other, less common infections. They all have common features. For example, such as a sharp increase in body temperature, vascular damage, intoxication and skin affects. The main route of transmission is insect bites, which are common in a particular area. In most cases, it is the skin that is the entry point for bacteria.
Tick-borne rickettsiosis is transmitted through blood-sucking parasites by the entry into the human blood of infected blood that contains the causative agent of the disease. Carriers are ticks and lice. In most cases, infection occurs through a bite. Sometimes infection occurs after rubbing the killed parasite carrier over damaged skin (for example, with scratches).
Several variants of the course of the disease are possible. The type of bacteria influences how it manifests itself. Some species are distributed only in subtropical climates. Others are in steppes or desert areas. Despite this, all pathologies have a similar clinical picture. Certain symptoms and characteristics help suggest a disease.
The infection has spread almost throughout the world. Moreover, each specific disease can only be found in a certain area. For example, epidemic typhus, known to mankind for hundreds of years. This disease was also called ship fever, as it mainly affected sailors and prisoners. Its causative agent is the bacterium R. prowazekii, which is transmitted through lice bites. A disease with similar symptoms, but caused by a different bacterium (R. typhi), occurs in regions with warm and humid climates. Often diagnosed in rural areas in summer.
Rickettsial diseases are infectious diseases that are found only in the habitats of parasite vectors. Almost all of these pathologies are zoonotic. Animals are an intermediate reservoir for the bacterium. While various types of ticks and body lice are carriers. The number of patients increases sharply in the summer, during the breeding season of these parasites. The infection poses the greatest danger to people who work outdoors (garden) and who are in contact with animals (pastures).
Cause of rickettsiosis
The etiological factor in the occurrence of the disease is a microorganism – rickettsia. This infectious agent can be classified as bacteria or viruses. This phenomenon is explained by the fact that, despite the structure of the microorganism (bacillus or coccus), rickettsia has the ability to intracellular parasitism. The pathogen is unstable in the environment. Rickettsia die when exposed to high temperatures or disinfectants. However, they can remain viable for a long time in cold and dry climates. In addition to the transmissible route of transmission, rickettsia can enter the body through blood transfusion or from the mother during childbirth. Some diseases in this group are characterized by other routes of infection. Among them are nutritional and airborne infections. Factors that provoke tick-borne rickettsiosis include:
- Contact with rural domestic animals, dogs.
- Lack of personal hygiene.
- Contact with infected people and carriers of pathology.
Epidemiology
Rice. 1. Curve of the monthly incidence of vesicular rickettsiosis in the Donetsk region (20-year average as a percentage of the annual incidence).
Incidence of V. r. characterized by spring-summer seasonality, although cases of V. r. are detected throughout the year: its increase begins in March - April, reaches a maximum in May, remaining at this level in June - August, then quickly decreases (Fig. 1). Seasonality of incidence of V. r. associated with the biology of the tick vector. The maximum increase in incidence coincides with the period of greatest tick activity. No dependence on the gender and profession of the sick has been established; among the sick, people aged 30 to 50 years predominate. V. r. is an “urban” infection, where it often affects individual areas, blocks, streets and houses, in which diseases are observed systematically, but are sporadic; family and group diseases are observed extremely rarely. The vast majority of patients have a history of contact with rats or mice at their place of residence or work. Studying the role of these rodents in the epidemiology of the disease, V. M. Zhdanov et al. (1950) isolated the pathogen after infecting a guinea pig with a mixture of mouse and rat brain suspensions. In parallel studies in the same area, S. M. Kulagin isolated 4 strains of rickettsia from house mice and 1 strain from gray rats caught in households where there were sick people. Consequently, the source of the causative agent of V. r. are house mice and gray rats. In the same outbreaks, 3 strains of the pathogen were isolated from A. sanguineus gamasid mites collected from mice and near mouse burrows in rooms where sick people lived. Thus, it has been established that the infection among rodents is spread by A. sanguineus ticks, which very often attack humans. Infection is possible when rickettsiae get into the wound when a tick sucks blood or when rickettsiae are rubbed into the skin when it is crushed.
Transovarial and transphase transmission of rickettsiae by ticks to offspring indicates that gamasid ticks are the guardians of the pathogen V. r. The role of other rodent ectoparasites in the transmission of the pathogen has not been established.
A. sanguineus is a burrow parasite, is polyphage and is associated with a wide range of hosts. The period of blood sucking lasts from several minutes to 36 hours, after which the tick leaves the host and hides in a shelter. Because of this, the reproduction and development of ticks depends not only on the presence of a host, but also on the microclimate of the shelter. The specific features of the tick's life cycle are determined by the constancy (daily and seasonal) of the host's stay in the shelter and the seasonality of changes in the microclimate of the shelter itself. The development cycle of A. sanguineus lasts 22-54 days and consists of a non-feeding larval phase and subsequent blood-sucking phases - two nymphal and one mature. The tick is characterized by its individual longevity (up to 1 year), with the ability to feed repeatedly up to 5-7 times and lay eggs after each feeding. At low temperatures, ticks can starve for up to 4 months. In human outbreaks, ticks are found on walls, floors and heating appliances, as well as in indoor garbage near burrows and in underground spaces near burrows.
Mechanism of disease development
The disease develops a few days after the tick penetrates the skin. The duration of the incubation period depends on the type of pathogen and the body's immune response. When a tick bites, a local reaction occurs. The skin becomes swollen, hyperemic, and painful. The infiltrate occurs due to the accumulation of immune system cells at the site of insect penetration. From there, the causative agents of the disease - rickettsia - penetrate into the lymphatic vessels and nodes. There they temporarily settle and reproduce. Considering that the lymph nodes belong to the organs of the immune system, they become noticeably enlarged. Cell activation and proliferation occurs to combat bacterial agents. Later, rickettsiae enter the blood vessels. Bacteremia and toxinemia occur. The veins and arteries of the skin are primarily affected. An inflammatory reaction develops in the walls of blood vessels, leading to destructive changes in the endothelium. In addition, rickettsiae often penetrate the arteries and veins of the brain. As a result, signs of central nervous system damage, meningitis and encephalitis, and possibly acute circulatory disorders develop. The mechanism of infection development determines the clinical picture of the pathology of tick-borne rickettsiosis. ICD-10 is an international classification that includes all diseases. This infection is no exception. In addition, pathological complications such as meningitis, encephalitis and vascular damage are coded separately in ICD-10. The main disease has code A77.
READ ALSO: Rash in the groin of a child: causes
How does infection occur?
Tick-borne rickettsiosis is a collective name for several types of diseases. This group of infectious diseases includes:
- Marseilles and Rocky Mountain spotted fever;
- Australian rickettsiosis;
- vesicular and paroxysmal;
- North Asian K. river;
- East African tick-borne typhus;
- typhus of North Asia.
Mostly all names reflect foci of infection.
On a note! In Russia, the greatest prevalence of tick-borne rickettsiosis is observed in the Siberian regions (southern Western and Eastern Siberia), as well as in the Far East and Northern Asia.
The causative agents of the disease are rickettsia. These microorganisms occupy an intermediate position between viruses and bacteria and are capable of parasitizing both in the cytoplasm and in the nucleus of cells. The carriers of the infection are ixodid, gamasid and red ticks, which become infected from rodents.
Interesting! The microorganisms were named after the American doctor Howard Ricketts; he studied them for several years and died in 1910 from typhus.
If a tick has rickettsiae in its body, it becomes invasive, and carriage can persist until the fourth generation. After sucking and biting human skin, the infection with the arachnid’s saliva penetrates the lymphatic tract and spreads through the bloodstream throughout the body.
Tick-borne rickettsiosis is characterized by seasonality, which is determined by the active season of ticks: from May to September. The highest peak occurs in May.
A tick bite is the most common method of infection. But there are other ways of transmitting rickettsial diseases (Q fever):
- when swallowing feces or urine of an infected animal or person (unwashed fruits, milk);
- when scratching the affected skin and rubbing rickettsiae;
- by airborne droplets.
Tick-borne rickettsiosis: symptoms of pathology
Despite the fact that tick-borne rickettsioses differ from each other, they all have common clinical manifestations. The incubation period averages from 3 to 7 days. Often, the penetration of mites into the skin goes unnoticed at the onset of the disease. Sometimes there is noticeable infiltration and regional lymphadenitis. Primary affect is characterized by compaction, in the center of which there is skin necrosis (brown color), and along the periphery - hyperemia (red rim). After 2-3 days, intoxication syndrome and persistent fever develop. The patient complains of body aches, fever up to 39 degrees, muscle pain, and general weakness. The febrile period is about 1-2 weeks. In addition to the symptoms of intoxication, rashes appear at the beginning of the disease. They have a roseolous-papular character. The rash first appears on the extremities and later spreads to the torso. The background of the skin does not change. These signs characterize tick-borne rickettsiosis. Photos of skin manifestations can be found in specialized literature. Distinguishing between rashes is very important for diagnosing infectious pathologies.
Rickettsial disease
Rickettsial diseases of the typhus group
Epidemic (lousy) typhus occurs with fever, intoxication, roseola-petechial rash on the skin, damage to the vascular and nervous systems.
The incubation period ranges from 5 to 21 days. Rickettsiosis manifests itself with an increase in body temperature and general intoxication symptoms, which reach maximum severity by the 3-6th day of the disease. During this period, marked hyperemia and puffiness of the face, injection of the sclera, and enanthema on the soft palate are noted. Approximately on the 5th day, a bright, characteristic roseola-petechial rash appears on the skin of the lateral surface of the chest, abdomen, and flexor surfaces of the arms. After a week, the rash turns pale, and disappears in the 2-3rd week from the onset of the disease. At the same time, the temperature decreases and intoxication disappears, but post-infectious asthenia persists for several more weeks. In severe cases of rickettsiosis, damage to the central nervous system occurs in the form of meningitis or encephalitis. Complications of epidemic typhus may include otitis media, mumps, pneumonia, and myocarditis. Brill's disease, or relapsing typhus, manifests itself with the same symptoms, but less pronounced. Endemic (rat or flea) typhus begins acutely and in the initial period is characterized by general infectious symptoms (fever, chills, arthralgia, headache). At the height of the febrile period, a rash appears on the chest, abdomen and limbs, which is predominantly roseolous-papular in nature. Characterized by arterial hypotension, bradycardia, general weakness, dizziness. In general, the disease is milder than epidemic typhus.
Rickettsial diseases of the spotted tick fever group
North Asian tick-borne rickettsiosis, or tick-borne typhus of North Asia, is transmitted through the bites of ixodid ticks. A typical sign of tick-borne rickettsiosis is the primary affect - the primary inflammatory reaction of the skin at the site of penetration of the pathogen. It is a painful compaction, surrounded by a zone of hyperemia and covered with a brown scab in the center. Simultaneously with the appearance of the primary affect, body temperature rises, regional lymphadenitis and intoxication syndrome develop. Skin rashes appear on the 2-3rd day and are represented by polymorphic roseolous-papular elements located on the body and around the joints. There is hyperemia of the face and pharynx mucosa, bradycardia, hypotension, and moderate hepatosplenomegaly. The course of North Asian tick-borne rickettsiosis is benign; usually by the 14th day of the disease recovery occurs.
Marseilles fever is also characterized by the presence of a primary affect at the site of tick penetration, fever, lymphadenitis, and maculopapular rash. The initial signs of rickettsiosis are similar to tick-borne typhus in North Asia. The primary affect looks like a dense infiltrate with central necrosis, which subsequently ulcerates and epithelializes only during the period of convalescence (after 3-4 weeks). Against the background of febrile intoxication manifestations, hyperemia of the oropharyngeal mucosa, sore throat, and conjunctivitis are expressed. The hallmark of Marseilles fever is a rash that affects not only the body, but also the face, palms and soles. Usually the rash is maculopapular in nature, but can transform into pimples (“pimply fever”) with hemorrhagic contents. The rash fades gradually, and pigmentation remains in its place for a long time.
Rocky Mountain spotted fever is a severe rickettsial disease. In the acute period, the disease is accompanied by chills followed by fever; severe headache and muscle pain, nosebleeds. Neurological changes include insomnia, impaired consciousness (stupefaction, prostration), convulsions, para- and hemiplegia, visual and hearing impairment. There is no primary affect. The rash with this type of rickettsiosis is profuse, petechial, and tends to merge to form large spots. The mortality rate from this rickettsiosis reaches 7%.
Paroxysmal rickettsial diseases
Paroxysmal rickettsiosis occurs with recurrent febrile attacks, repeating every 5 days (with Volyn fever) or 2-3 days (with paroxysmal tick-borne rickettsiosis). During an attack, the temperature rises to 39.0–40.5°C, chills, ossalgia, myalgia, arthralgia, and headaches appear. Primary affect, skin rashes and regional lymphadenitis are not constant companions of paroxysmal rickettsial infections and are often absent. The course of fevers is usually protracted, but benign.
Detection of tick-borne rickettsiosis
You cannot rely solely on the clinical picture to identify tick-borne rickettsiosis. Diagnosis of the disease should include laboratory tests. After all, the symptoms of the pathology can resemble many other infections. To make an accurate diagnosis indicating the type of pathogen, serological studies are carried out. Among them are enzyme immunoassay, complement fixation reaction, hemagglutination, etc. Microscopy of blood, cerebrospinal fluid, urine and discharge infiltrate is also performed.
READ ALSO: How to get rid of wen on the face: TOP 10 remedies
Routes of infection
You can become infected with a disease such as tick-borne rickettsiosis only after being bitten by a tick that is the carrier of the infection, or as a result of rickettsia getting into an open wound surface. Typically, wild rodents are the reservoir and carrier of the infection, since their disease is asymptomatic. But the urine of sick cows and their feces can also pose a danger to humans, which is why very often a disease such as tick-borne rickettsiosis occurs among farm workers.
Tick-borne rickettsiosis is the most common disease, as it is transmitted by ticks. Rickettsia can persist for a long period of time in the salivary glands of the insect. Mushroom and berry pickers, as well as lumberjacks and people associated with the woodworking industry are especially susceptible to this disease.
Tick-borne rickettsiosis: treatment of infection
Since the disease is a bacterial infection, treatment requires the use of antibiotics. For this purpose, the drugs “Tetracycline” and “Levomycetin”, as well as their analogues, are used. In severe cases of the disease, the patient should be hospitalized in an infectious diseases hospital. For the purpose of detoxification, a solution of 5% glucose with ascorbic acid is administered intravenously. For bradycardia, it is necessary to use vasopressor drugs. These include medications “Atropine” and “Caffeine”. Symptomatic therapy is also carried out - antipyretics, antihistamines. Ticks are removed using tweezers. If complications develop, specific treatment is carried out.
Prevention of tick-borne rickettsiosis
Nonspecific prevention includes the control of insects and rodents, as well as compliance with personal hygiene rules. Vaccinations are carried out against typhus and Q fever. If a disease is detected, it is necessary to sanitize the premises, as well as examine all persons who were in contact with the patient. If the tick has already penetrated the skin, but symptoms of infection have not developed, emergency drug prophylaxis is performed. The antibiotics Doxycycline and Azithromycin are used.
News MirTesen
Prevention of rickettsiosis
Prevention of rickettsiosis includes a whole range of measures, which include not only individual human protection, but also veterinary and agrotechnical methods. An important stage is the person’s own compliance with individual protective measures against various rodents and ticks, as well as compliance with basic rules of personal hygiene and sanitary standards in places of residence to prevent lice infection. If a person is in places where there is an epidemic risk of ticks, you need to protect yourself with special clothing or try to use things that fit tightly to the body and protect against bites. Often they use overalls impregnated with special chemical solutions, tick repellents, and Pavlovsky nets. A very important point in self-defense is a careful examination of a person’s skin after returning from the street or from the forest for the detection of blood-sucking arthropods. If they are identified, it is recommended to either seek medical help for their proper removal, or remove them yourself by treating the bite site with medical alcohol or iodine. The removed tick must be taken to the sanitary and epidemiological service for examination. Timely administration of preventive treatment in the form of taking Doxycycline or Azithromycin will help reduce the risk of infection and the development of complications.
It is important to always carry out rodent control if detected, and carefully protect food and water from possible contamination with their waste. Meat and dairy products, which can also cause infection with certain types of rickettsioses, must always be well-heated
When identifying a patient suspected of being infected with any type of rickettsiosis, it is necessary to initially isolate him, identify contact persons and be sure to carry out sanitary treatment in his place of residence.
Vaccines that could be used as an emergency or preventive means of protection against rickettsial infections have not yet been developed. Only to protect the population from Q fever has a specific vaccine been created from Burnet's rickettsia, which can be used to create immune protection among the population in areas of its spread. An important stage is the active conduct of sanitary and epidemiological work, lectures, educational conversations among the population of epidemically dangerous areas, to familiarize themselves with the basic rules for preventing infection, types of diseases, emerging symptoms and protective measures.
Rickettsiosis - which doctor will help? At the slightest suspicion of infection with rickettsiosis, you should immediately consult a doctor such as an infectious disease specialist.