Tick-borne encephalitis
Tick bite
Borreliosis
8168 11 November
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. We remind you that independent interpretation of the results is unacceptable; the information below is for reference only.
Ixodid tick research: indications for use, rules for preparing for the test, interpretation of the results and normal indicators.
Carrying out a blood test for borreliosis
Tick bites pose a considerable danger to our health, and therefore the test procedure for borreliosis is mandatory after such incidents.
Ticks often appear in urban areas, so you should be especially attentive to your own health. Many people remember that ticks are carriers of encephalitis, but in addition to this dangerous pathology, they are capable of transmitting many other infectious pathogens. That is why analysis for borreliosis is mandatory. There are a huge number of possible research options.
Norm and interpretation of results
In laboratory test forms for borreliosis, a quantitative (in numbers) or qualitative (yes, no) result is indicated. Decoding the diagnosis of borreliosis for IgG antibodies looks like this:
- less than 10 units per ml (negative) – there is no infection or blood was donated early;
- 10-15 units per ml (doubtful);
- more than 15 units per ml (positive).
The results of the IgM antibody test look like this:
- up to 18 units per ml (negative);
- 18-22 units per ml (doubtful);
- more than 22 units per ml (positive).
After 2 weeks, it is recommended to take tests for borreliosis again.
The immunoblot result is visible on the test membrane. The stripes that appear indicate the absence or presence of antibodies to the antigens. Opposite the strip indicating the antigen, the laboratory technician writes a “+” or “–” sign. In conclusion, they write that the result of the test for borreliosis:
- positive;
- negative;
- indeterminate (if the stripes appear very weakly).
The immunoblot must be taken again after a month and a half.
The form with the result of the PCR analysis indicates whether Borrelia genetic material was detected or not.
The normal test result is negative. The outcome of the diagnosis of borreliosis may be affected by treatment with antibiotics (you must notify the doctor about this in advance), as well as other diseases:
- mononucleosis;
- HIV;
- syphilis;
- typhus (relapsing);
- autoimmune pathologies.
Briefly about borreliosis
This pathology is caused by extremely small spiral-shaped microorganisms. Most often, Borrelia infection occurs in late spring and early summer in park and forest areas.
After being bitten by ticks that carry a pathogenic microorganism, the latter penetrate through all layers of the skin to the vessels, and then spread through the bloodstream throughout the body. Most often there is an acute form of the disease, which is characterized by:
- Severe headaches;
- The appearance of ring-shaped erythema at the sites of bites;
- Sore and sore throat;
- Cough symptoms and runny nose;
- Low-grade fever up to 38 degrees;
As you can see, Lyme disease, which is caused by this microorganism, can be easily confused with ARVI or the influenza virus. Often, patients independently carry out symptomatic treatment, unaware of the true cause of the disease.
It is important to carry out diagnostic measures on time to exclude further development of the pathological process. Remember that the immune system can rarely cope with bacteria on its own, so it is important to carry out timely antibiotic therapy.
Fortunately, today there are a number of efficient, fast and effective diagnostic methods that can provide accurate results in a matter of hours or days. All these measures have made it possible to significantly reduce the number of borreliosis and deaths over the past decade.
Lyme disease treatment
Lyme borreliosis is treated in an infectious diseases hospital. It is based on complex drug etiotropic and pathogenetic therapy, taking into account the stage of the disease. The basic drugs at the first stage of the disease are tetracycline antibiotics ( Doxycycline , Tetracycline ).
Treatment of borreliosis with antibiotics after a tick bite in cases of contraindications (pregnancy, children under 8 years of age) is carried out with beta-lactam antibiotics ( Cefuroxime , Amoxicillin ), and in cases of an allergic reaction to them - with macrolides ( Azithromycin , Clarithromycin ). In the second and third stages, the main drugs of treatment are Ceftriaxone , Cefotaxime .
Penicillin in massive doses. In this case, antibiotic therapy must be continued for 21-28 days.
How to continue treatment of borreliosis after a course of antibiotics? Treatment after a course of antibiotic therapy is determined by clinical manifestations and their severity. For example, for general infectious symptoms, detoxification therapy is prescribed; for meningitis - dehydration therapy is carried out ( Furosemide , Reogluman ); for arthritis - analgesics ( Paracetamol ), NSAIDs ( Indomethacin , Piroxicam ), drugs that improve neuromuscular conduction ( Oxazil , Proserin ) and so on. It should also be taken into account that after a course of antibiotics, the development of dysbacteriosis , candidiasis , and pseudomembrane colitis .
In order to prevent them, it is recommended to consume fermented milk products such as acidophilus , prebiotics and probiotics, vitamins, especially group B. It should be said that treatment with folk remedies, which are offered on various forums (forum for patients with Lyme disease, vivo forum, etc.) is not recommended, since the prognosis of the disease clearly correlates with the early stages and adequacy of antibacterial therapy. In extreme cases, they can be considered as an additional remedy to antibiotic therapy.
Polymerase chain reaction
A blood test for borreliosis using PCR technology allows you to obtain comprehensive information about the pathogen. This technique is based on determining the genetic information of the pathogen. The accuracy of its results reaches almost one hundred percent.
Blood for borreliosis can be taken in almost any laboratory. This method is different:
- Manufacturability of collecting material for analysis;
- High reliability of results;
- High sensitivity;
- Allows you to determine the number of pathogens;
The material for PCR can be not only the patient’s blood, but also lymph, cerebrospinal fluid and even tissue from the biting tick. Analysis of a tick allows not only to determine its type and pathogenicity, but also the presence of other microorganisms that may pose a health hazard.
PCR results provide accurate results in just 24-72 hours, while standard bacteriological analysis requires about 8-10 working days. In addition, with borreliosis, antibodies are released to borrelia, which initiate an immune response. After a bite, antibodies to borreliosis of the IgM class are released.
The interpretation of the PCR analysis of borreliosis is quite simple - “positive” or “negative”, which indicates the presence of the genetic apparatus of the infectious agent in the material being studied. A positive result indicates that Lyme disease will develop to its maximum in the near future, and therefore it is necessary to begin appropriate therapy.
This technique makes it possible to separate encephalitis and other infectious agents from borelliosis. PCR allows you to do this directly during the main procedure.
What about borreliosis?
A blood test for borreliosis is important because there is no vaccine for the disease. In addition, a person does not develop a stable immunity to the bacterium, he can get sick again.
Lyme disease occurs in humans after the Borrelia bacteria enters the body. It is immediately attacked by the immune system and moves to places where the immune system cannot cope - in the heart, nerve tissue, tendons. For this reason, unlike encephalitis, the acute stage is not observed, and the disease becomes protracted. The main distinguishing symptom is migrating annular erythema, which looks like a bright red spot at the site of the bite, gradually growing in size and forming rings. The skin peels off and necrosis appears. Erythema of an allergic nature may also appear on other parts of the body. In some forms of the disease, they may be absent altogether, but intoxication and fever appear, which makes borreliosis almost indistinguishable from encephalitis. A blood test for tick-borne borreliosis and encephalitis will help differentiate the disease.
A month later, symptoms of central nervous system damage appear: partial paralysis of the limbs, speech disorders, mood swings. Meningitis may develop. If no action is taken, after a year arthritis, hearing loss, neuralgia, disorientation, and severe speech defects begin to progress.
The carriers of the class of bacteria to which Borrelia belongs are the same ticks that transmit encephalitis. The causative agent of Lyme disease lives in the digestive system of the tick, and not in its saliva, so it does not spread in the human body immediately. If the insect is removed in a timely manner, there is a chance of not becoming infected.
Borreliosis can be treated, the main thing is to avoid transition to the chronic stage. The patient is prescribed medications, the correct use of which guarantees recovery.
Lyme disease is not transmitted from person to person, but there is a possibility of transmission from a pregnant woman to her fetus. That is why this disease is sometimes diagnosed in newborns.
A blood test for borreliosis and encephalitis can be taken in infectious diseases hospitals, commercial and virology laboratories. The main thing is that the clinic conducts parallel studies of both diseases.
ELISA (enzyme-linked immunosorbent assay) procedure
Despite the fact that immunoblot for borreliosis allows you to obtain more reliable information, ELISA is a rapid method that shows how the level of IgM in serum changes. This test requires you to donate blood for antibodies after a bite to find out your own indicators.
Materials for analysis for tick-borne borreliosis are taken twice, with an interval between samples of 21-28 days after the bite. In addition, the titer (increase in the amount of IgM) antibodies will indicate the intensity of the infectious process.
The accuracy of the result depends on many factors. For this reason, it is necessary to adhere to some rules when taking the appropriate analysis:
- Avoid stressful and physical activities shortly before the test;
- Do not consume alcohol, fatty or spicy foods 72 hours before the test;
- Try to reduce the amount of pharmacological drugs used;
- Testing after ultrasound, x-ray diagnostics and physical procedures is not acceptable;
- Try not to smoke on the day of the test;
- The test is taken on an empty stomach;
As you can see, there are really a lot of rules. It is important to adhere to them, since the result of the Barreliosis analysis can vary due to many factors. Tick-borne borreliosis must be correctly diagnosed so that the correct treatment can be prescribed.
Remember that an incorrect diagnosis (eg encephalitis) will lead to an incorrect diagnosis and loss of time.
Bacteriological (cultural) methods
Such studies do not use an immunochip or a series of serological tests. The disease is diagnosed by isolating the pathogen on nutrient media and then examining it.
To determine the type of Borrelia, light and other types of microscopy are used, as well as a number of biochemical reactions, the assessment of which allows us to draw meaningful conclusions, distinguishing encephalitis from borreliosis.
The presence of a pure culture allows testing for antibiotic sensitivity and resistance. Absolutely all microorganisms and bacteria change at high speed, acquiring new unique properties, and only their careful study makes it possible to identify changes.
Various tissues and body fluids (blood, cerebrospinal fluid, intra-articular, lymph, etc.) are ideal for cultivation. This type of microorganism is extremely demanding on the cultivation environment, so special media are used in bacteriological laboratories.
To obtain accurate results, you must follow a number of rules and regulations:
- Biomaterial should be obtained in the early stages of disease development;
- Maintain sterility during material collection;
- Quick transfer to the bacteriological laboratory to begin cultivation;
Such studies have relatively low impact with a lot of work involved. The immunochip allows you to get results much faster and more accurately. The study data changes significantly if the patient began using antibiotics shortly before the analysis.
Of course, this method has the right to exist in medicine, but its effectiveness is very low. It is much more effective to use more modern diagnostic methods. Bacteriological research is suitable for scientific experiments in theoretical medicine and various research institutes.
Advantages of the method
An immunochip for determining borreliosis has several advantages over others, including serological tests for this disease. The main advantages include:
- the ability to determine a wide range of antibodies of classes G (IgG), M (IgM) to various types of bacteria that cause borreliosis;
- accuracy of determining the amount of antibodies;
- the ability to evaluate not only the qualitative composition of antibodies, but also their quantity based on the positivity rate;
- the ability to identify the duration of infection with borreliosis;
- high sensitivity;
- ease of execution;
- automated interpretation of results, which eliminates the subjectivity of the assessment;
- A small amount of the test material is taken for analysis.
RIF analysis
A fairly fashionable and modern diagnostic method is radio enzyme immunoassay. The complementary antibody or enzyme is labeled with a radioactive ion (iodine or bromine), and then the material being tested is processed.
The next step is to wash the test materials to remove uncombined enzymes. Using dark-field microscopy, a greenish or blue glow is visible, which is a positive result of this test.
The method is quite fast and inexpensive, which allows you to get results in the shortest possible time. In addition, this method allows you to determine even the presence of individual components of the cell wall, which indicates the presence of an active cellular immune response.
This method is quite informative, but recently it has increasingly been replaced by more modern technologies.
When should you conduct an examination?
It has been repeatedly mentioned that each method has its own advantages and disadvantages, and has a number of limitations on its application. It is for this reason that there are certain deadlines for collecting material for each method.
The polymerase chain reaction should be carried out only 10-12 days after the bacteria are supposed to enter the patient’s body, and ELISA and RNIF reactions can be carried out only after a month.
All these features must be taken into account when diagnosing, and only an experienced infectious disease doctor can present the full picture. Remember that prescribing diagnostic procedures on your own may lead to incorrect results, which may cost you your health.
After a tick bite, you should seek advice from a medical clinic or personally to the necessary doctor. He will prescribe a collection of material (most often venous blood) for analysis, and will also recommend the appropriate laboratory.
Remember, it is much easier to prevent borreliosis than to treat it. When in forest or park areas, use anti-tick products, wear thick clothes and hats. These primitive means significantly increase your safety.
Blood test for borreliosis after a bite
Tick bites carry great danger, and this concerns not only possible inflammatory reactions, but also the danger of contracting a serious disease called borreliosis. During the active period, parasites can appear even in urban areas, so be especially careful in the spring season.
After a bite, it is worth taking a blood test for borreliosis, since the disease is characterized by a high rate of development. Today there will be no problems with obtaining accurate analyzes.
Features of borreliosis and encephalitis
Encephalitis and borreliosis (Lyme disease) are transmitted by ticks in Russia. These infectious diseases are often confused, although they are fundamentally different. Tick-borne encephalitis is viral in nature, while borreliosis is bacterial. Both diseases affect the central nervous system, but Lyme disease also affects the joints, heart muscle and skin. Encephalitis is characterized by an acute form, while borreliosis is characterized by a chronic course. As each disease develops, it receives distinct differential symptoms. A blood test for encephalitis and borreliosis will help determine infection.
Interpretation of tests for borreliosis
Below you can see the transcript of the results:
- If the amount of antibodies in the blood plasma is less than 0.8 U/ml, or they are completely absent, this is an indication that the patient has not been infected with borreliosis.
- When the antibody level is from 0.8 to 1.1 U/ml, then such an analysis is classified as doubtful. It is impossible to make an unambiguous decision, so a repeat analysis is usually prescribed to confirm the diagnosis or refute it.
- If antibodies to Borrelia are at a level of 1.1 U/ml and above, then the diagnosis is confirmed and a course of treatment is prescribed.
In the case when, after taking the test, only IgG antibodies were found in the blood, this is an indication that the person has already been infected with borreliosis before. Or he was vaccinated against a disease of this type. Immunoglobulins of this type can remain in the human blood for a long time, even after complete recovery has occurred.
Decoding
The results of the analysis for IgG antibodies are given in quantitative terms with the appearance in the decoding of the concept “titer” - an indicator of the concentration of antibodies (for example, 1:100, 1:400, etc.). If it is more than 1:100, then the immune system is reacting. If it is less, then this shows a lack of reaction, and if the virus penetrates, the person will definitely get sick. The indicator of a healthy body is from 200 to 400.
The results of a blood test for IgM antibodies are qualitative: whether detected or not. If there are IgG levels in the blood and no IgM, such results most likely indicate vaccination. And the presence of both indicators indicates infection. The test should be repeated in a week to establish an accurate diagnosis.
When to get tested for borreliosis after a bite?
You should not rush to get tested for tick-borne encephalitis and borreliosis immediately after a tick bite. The fact is that in the early period the analysis will not be sufficiently informative. When using the PCR method, blood can be tested no earlier than 10 days after the parasite bit you. Testing for antibodies to Borrelia is carried out even later - after 3-4 weeks.
Erythema after a tick bite infected with borreliosis
It can be very informative for specialists to study the tick itself that bit the person. The difficulty here is that often people forget that the parasite itself can be very helpful in making an accurate diagnosis.
If you don’t know where you can donate blood for borreliosis, then just contact any clinic in your city. However, check whether the chosen institution tests for borreliosis. The fact is that some clinics specialize only in detecting encephalitis. The problem is that ticks can carry two diseases at once.
There are no serious preparation requirements before taking tests for borreliosis, but to increase the accuracy of the results it is worth following several recommendations:
- 7 hours before the test it is better not to eat anything;
- It is forbidden to drink alcohol the day before the procedure;
- It is better not to smoke half an hour before blood sampling.
In rare cases, additional cerebrospinal fluid testing may be needed to determine the disease. This method is not suitable for everyone, as it has contraindications. The procedure is quite painful.
What happens to the body after infection?
The disease can be detected within 6-12 days. Thanks to clinical studies, it was possible to learn how to determine the early and late periods of development of borreliosis.
- At the first stage of spread, skin and general infectious symptoms are observed.
- The second stage occurs 2-4 weeks after the infected tick bites a person. During this period, the virus spreads throughout the body.
- The third stage can occur either a few months after infection or years later. Most often this is a chronic disease.
IgM antibodies to Borrelia burgdorferi
Serological indicator of early stages of infection with Borrelia spirochetes.
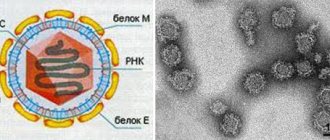
Borreliosis or Lyme disease (named after the place where the disease was first identified in 1975) is a common tick-borne infection. The causative agent is a very small spirochete Borrelia burgdorferi, the only Borrelia pathogenic for humans. The hosts are many vertebrates: dogs, sheep, birds, cows and horses, but the main host and vector are ixodid ticks, in which the infection lasts throughout the life of the tick. In Russia these are I.ricinus and I.persulcatus. The disease is typical for the spring-summer period. It is more often observed in the Moscow, Leningrad, Tver and other, mainly northern regions, as well as in the Baltic states.
The disease is systemic, having 3 stages:
- Stage I occurs one week after the tick bite and lasts from 3 to 33 days. It is characterized by fever and erythema migrans. If therapy is started at this stage, then further development of the disease can be prevented.
- 4 weeks after the bite, stage II develops. It is characterized by cardiac damage and a neurological “triad”: aseptic meningitis, facial paralysis and peripheral neuropathies.
- After 6 weeks, and sometimes after several years, untreated patients develop severe joint damage.
Laboratory diagnostics. With the classic picture of erythema migrans, the diagnosis is made based on clinical signs, in other cases it is confirmed by laboratory methods. Culture, detection of pathogen antigen and histological examination of the skin are not sufficiently sensitive and specific; histological examination is, in addition, invasive. Therefore, the diagnosis is confirmed mainly by serological methods - detection of specific IgG and IgM antibodies to the pathogen in the blood (in the INVITRO laboratory, tests No. 243 and 244, respectively).
PCR testing for the presence of genetic material of the pathogen in this case is ineffective, but is used if necessary in patients with negative results of serological tests, but strong clinical suspicions of infection, as well as in patients with immunodeficiency.
Specific antibodies to Borrelia burgdorferi begin to be detected 2-4 weeks after the onset of infection (first IgM, then IgG), the maximum amount of IgG is synthesized 1.5 - 3 months after infection. Antibodies to Borrelia burgdorferi are often not detected in the early, localized stage of the disease or when antimicrobial therapy is started early. Thus, a negative result of serological tests in the early stages of infection does not confirm its absence and requires re-checking over time after 2 to 4 weeks. At the disseminated and chronic stages, specific antibodies to the pathogen are almost always present.
IgG antibodies circulate in the blood for a long time (from several months to several years), even after successful antimicrobial therapy and cure of the infection. Therefore, the success of treatment cannot be judged by the presence and titer of antibodies. Immunity against Borrelia burgdorferi is not sterile. People who have been ill may become infected again after a few years. The detection of antibodies to Borrelia burgdorferi is not always accompanied by clinical signs of Lyme disease.
It is estimated that the specificity of ELISA testing for antibodies to Borrelia burgdorferi currently reaches 95% (i.e., nonspecific reactions, cross-reaction with antigens of other bacteria can give false-positive results in approximately 5% of cases). In doubtful cases, immunoblotting is used to confirm the results of ELISA tests.
Antibodies to the causative agent of borreliosis IgG (Lyme disease) (in the blood)
Key words: Lyme BL tick-borne borreliosis ixodid tick ixodid borreliosis blood
Antibodies to the causative agent of borreliosis IgG in the blood (Tick-borne systemic borreliosis or Lyme disease) are an indicator of infection with the spirochete Borrelia burgdorferi after a tick bite. Main indications for use: confirmation of the diagnosis of Lyme disease (borreliosis), a clinical picture similar to borreliosis (fever, erythematous migratory rash, symptoms of aseptic meningitis, neurological disorders, arthritis of unknown etiology and others).
Lyme disease (systemic tick-borne borreliosis) is a recurrent vector-borne infection caused by the spirochete Borrelia burgdorferi. The disease occurs in stages. Early manifestations include: headache, fever, fatigue, and a characteristic ring-shaped redness on the skin (erythema migrans). The first stage after a tick bite develops after a few days (up to a month) and occurs with fever and an erythematous migratory rash, occurring in 60-80% of patients. The second stage begins after 4 weeks and manifests itself in 10-15% of cases with neurological and cardiac symptoms (peripheral neuropathy, aseptic meningitis, heart pain, palpitations). The third stage (late period) develops after six months (and up to several years) with signs of arthritis in 10% of patients.
Borreliosis or Lyme disease is named after the geographic location of the area (Lyme, Connecticut, USA) in which the disease was first discovered in 1975. The disease occurs in North America, China, Japan, Australia, as well as in the countries of Eastern Europe, Russia, Moldova, and the Baltic states. The carrier is ticks. The causative agent of the infection is the spirochete Borrelia burgdorferi. The source of infection is many species of wild and domestic animals (including rodents and birds). An infected person is not a source of infection for another person. The mechanism of transmission of the pathogen is transmissible - through a tick bite. The main vectors of infection in European territory are ticks Ixodes ricinus and Ixodes persulcarus. These ticks (depending on the region) can also be carriers of another disease - Far Eastern tick-borne encephalitis (spring-summer encephalitis), which is caused by an RNA virus from the Togaviridae Flavivirus family. In the United States, the main vector of the spirochete Borrelia burgdorferi is the Ixodes dammini tick. The incubation period takes from 2 to 32 days. The initial stage of the disease, lasting up to 4-5 weeks, is characterized by fever, malaise and muscle pain. At the site of the tick bite, erythema develops, increasing in size (on average after 7 days).
Symptoms of Lyme disease
Lyme borreliosis is a systemic disease that develops in stages (stages), in accordance with the chronology of organ damage. In this case, the stages of the disease can occur sequentially or partially overlap one another. The stages are determined by the main clinical manifestations, the predominant involvement of organs in the pathological process, or by the duration of the disease. The incubation period of the disease varies from 2-3 days to 30 days, on average it ranges from 12-14 days after a tick bite or detection of a barley tick on the body.
Symptoms of borreliosis in humans after a tick bite develop gradually in most patients. As a rule, at the site of a tick bite in adults, redness or a papule appears, which over the course of several days gradually increases in size and expands, forming an erythema with a diameter of 10–15 cm, but its size can vary from 5 to 60 cm. Erythema migrans is one of the characteristic and most important pathognomonic signs of tick-borne borreliosis, which can be located in any part of the body, but is more often found on the hips, torso, and armpits (photo of symptoms below).
Often, patients at the site of tick suction at the end of the incubation period note slight itching, less often pain. The shape of the erythema is often round/oval with a hyperemic outer edge and a slight elevation above the level of healthy skin. In some cases, a crust remains in the center of the erythema (at the site of the primary affect). The severity of the disease does not depend on the size, shape and location of the erythema.
Sometimes, in addition to erythema at the sites of tick suction, similar skin manifestations appear on other parts of the body, which is due to the migration of borrelia by the lymphogenous/hematogenous route from the primary focus. Secondary erythema is characterized by the absence of primary affect and smaller size. As a rule, erythema, if left untreated, lasts 3-4 weeks and gradually disappears. In its place, hyperpigmentation, peeling of the skin, tingling sensation, itching, and decreased pain sensitivity are often observed.
In 60-70% of cases, erythema is accompanied by symptoms of general intoxication: general malaise, weakness, fatigue, regional lymphadenopathy , myalgia , respiratory manifestations, arthralgia , fever up to 37-38 ° C, less often - headache, chills, nausea and vomiting. In cases of non-erythema forms, infectious intoxication is the leading syndrome in the initial period. The duration of the febrile period, as a rule, does not exceed 15 days.
Borreliosis in adults at the second stage of the disease, which develops 3-10 weeks after the acute period, is characterized by symptoms of organ damage to internal organs (heart, liver), central/peripheral nervous system ( neuroborreliosis ), joints and eyes ( ophthalmic borreliosis ). Neurological manifestations vary widely, but in most cases, damage to the nervous system manifests itself in the form of radiculoneuritis , neuritis of the facial (cranial) nerves and meningitis with their characteristic symptoms. Neuroborreliosis is often manifested by combined symptom complexes of these syndromes.
Cardiac disorders are usually observed from 4-5 weeks of onset of erythema, which include changes in intraventricular and atrioventricular conduction, atrial fibrillation. Patients complain of breath , palpitations, sensations and pain in the heart area, dizziness .
Physically - an increase in the size of the heart, bradycardia , muffled heart sounds, systolic murmur at the apex of the heart. The duration of cardiac disorders does not exceed several weeks.
With articular syndrome, the frequency of which is 2-10%, arthritis , most often in large joints: knee (up to 50%), shoulder (up to 30%, elbow/ankle (20-25%). The degree and severity of changes in the joints are characterized by dynamism Patients complain of pain in the joint area, swelling and limited mobility.
The intensity of inflammatory changes is predominantly moderate with a mild exudative component.
Symptoms of borreliosis in adults at the third stage are characterized by a chronic inflammatory process and destructive manifestations. The main forms of this stage in adults include: neuroborreliosis in the form of progressive encephalomyelitis , polyneuritis , meningoencephalitis ; dermatoborreliosis ; mono- and polyarthritis .
The chronic course of Lyme disease (clinical manifestations persist for 6 or more months) is characterized by the progression of the inflammatory process mainly in the skin, nervous system or joints, less often in other organs, leading to atrophic/degenerative changes. In a chronic course, there are both variants of a continuous progressive course without remissions, and variants of a relapsing course with varying durations of periods of remission.
In this case, one leading syndrome comes to the fore, most often damage to the nervous system, skin joints or heart, and less often to other organs. Damage to the central nervous system is manifested by rapid fatigue, headache , sleep disturbance, and memory loss, which corresponds to the clinical picture of asthenovegetative syndrome. Then symptoms of multiple sclerosis , encephalomyelitis , mental disorders, and sometimes epileptiform seizures, may develop.
Below is an algorithm for determining the variant of the clinical course of Lyme disease.
Borreliosis test result
No. 35 761 Infectious disease specialist 08/12/2016
Please tell me what the analysis result means and what to do with it? The erythema was 6 weeks ago, and the tick bite was 2 months ago. The laboratory website states: Reference limits: >1. 0 CP – positive Maria, Krasnodar
ANSWERED: 08/12/2016 ANSWERED: 10/12/2017
18+ Online consultations are for informational purposes only and do not replace a face-to-face consultation with a doctor.
User Agreement Your personal data is securely protected. Payments and site operation are carried out using the secure SSL protocol.